The retina is a layered structure at the posterior region of the eye, comprising ten different layers and three different cell types. Photoreceptor cells- rods and cones- also known as retinocytes, are responsible for gathering and transducing light signals. They are pivotal for visual ability. These cells communicate with different retinal cells to transform light signals into nerve transmissions, which the brain can interpret. Retinocytes are implicated in several disorders, becoming central to ophthalmic research. Their in vitro culture has facilitated the understanding of the pathology behind visual disorders and the generation of suitable therapeutics. This blog explored the biology of retinocytes, their culture, and applications in biomedical research.
Primary Retinocytes
Distinguished into rod and cone cells, all retinocytes have similar morphological characteristics. They consist of a cell body, inner segment, outer segment, and axon (Fig 1). The cell body contains the nucleus, and it extends its axon into the outer plexiform layer of the retina. The inner segment has prominent endoplasmic reticulum and mitochondria. This segment is also the site of photopigment synthesis. Cilium connects both the segments. The outer segment contains photopigments, and it interacts with the processes of the retinal pigment epithelium (RPE). The orientation of this segment is towards pupils to augment the absorption of incoming light signals and enhance visual capacity.
Cones
Cone cells are responsible for daytime or phototopic vision. They concentrate towards the central region of the retina-macula, with the fovea consisting of 100% of cone cells. Their high density at the fovea allows for differentiating between two points. They share an equal ratio with the connecting ganglion cells, which confers high visual acuity. These cells employ the glutamate neurotransmitter to relay signals. Their photopigment opsin has three different subtypes S, M, and L that aid in the detection of various wavelengths of light. Opsin is a light-sensitive GPCR linked to 11-cis-retinal chromophore covalently through a Schiff base. Photon absorption changes the configuration of the chromophore into 11-trans-retinal, which causes a conformational change in the opsin protein, initiating the signaling cascade.
Rods
About 95% of photoreceptors in the retina are rod cells, conferring low light or scotopic vision. Their density is higher in the outer region or periphery of the retina. Unlike the comparable ratio of cone cells with retinal ganglion cells, rod cells converge into a single ganglion. This results in a slow response of rods and their low sensitivity to contrast and spatial acuity. But, this ratio also grants them higher sensitivity to single photons, a reduction in the background noise, and signal integration for more extended periods. Both photoreceptors are momentarily rendered inoperable by the photobleaching impact of daylight. Compared to cones, functional recovery takes longer for rods.
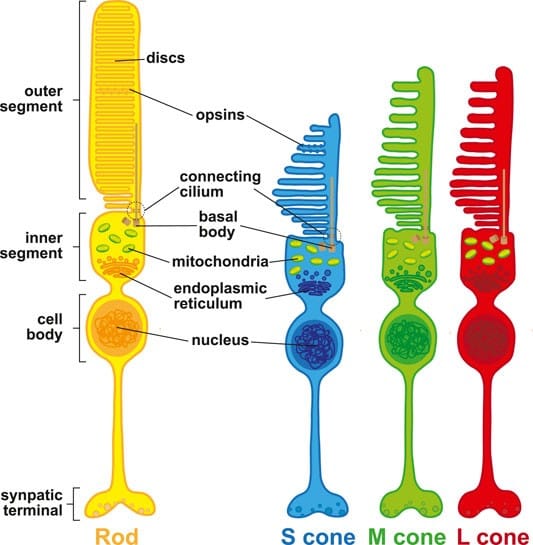
Figure 1. Morphology of rods and cones. S, M, and L cones indicate the different opsins present in each cell to detect small, medium and large wavelengths. (Image: PMID: 35493094)
Culture of Primary Retinocytes
The isolation of retinocytes follows the extraction of the eyeball from the donor and slowly removing different layers like the choroid, sclera, lens, etc. Digestion by papain dissociates Primary Retinocytes. Cell dissociation from the fovea region yields a high concentration of cone cells. Magnetic activated cell sorting (MACS) enhances the purity of the cell population. Rod-specific markers (CD73, rhodopsin, and recoverin) and cone-specific markers (opsin and peanut agglutinin lectin) are used for cell characterization.
The optimal culture media include DMEM (with or without F-12) or Neurobasal medium. Supplementation with N1, taurine, B27, and retinoic acid supports cell growth and maturation. Additionally, research studies have also coated the surface of culture vessels with materials such as gelatin, fibronectin, or poly-D-lysine. The media is changed under dim red light every 2-3 days. In the first few days of culture, processes of retinocytes become visible.
Applications of Retinocytes
Disease Pathogenesis
Several eye disorders are associated with retinocytes. For instance, color blindness occurs due to a deficiency of cone cells, a genetic mutation in these cells results in Usher syndrome, and inadequate development of rods results in night blindness. A study revealed that the liquid crystal display of computers and phones causes excessive blue light exposure. It subsequently leads to increased oxidative stress and photochemical damage to chromophores. Combined with age-induced decrease in antioxidants, the high levels of reactive oxygen species (ROS) result in age-related macular degeneration (AMD). Therefore, researchers are studying these cells to identify the key disease mechanisms and develop therapeutics. The culture of primary retinocytes also provides a platform for high-throughput screening of these therapeutics for efficacy and toxicity.
Transplantation
Degeneration of retinocytes is an irreversible process. For years, scientists have adopted the cell therapy approach. It involves transplanting healthy cells into the subretinal space to engraft and form neural connections with the retina for restoring vision. Although studies have reported visual recovery by this therapy, the mechanisms seem elusive. Some studies have demonstrated that the transplanted retinocytes do not integrate into the retina but rather transfer their cytoplasmic constituents to the host retina. This process is termed material transfer. Studies have shown the bidirectional nature of this process, requiring direct cell contact. Further research can divulge the transplant mechanisms as well as enable the selection of an appropriate source of retinocytes among tissue or Stem Cell derived retinocytes.
Development
The morphogenesis of different retinal cells, including retinocytes, has been a subject of investigation. Embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) have played a vital role in gaining knowledge about this process. Factors like OGF1, DKK, and noggin induce the transformation of ESCs in culture to retinocytes. The organoids generated from ESCs or iPSCs follow patterns of differentiation similar to those in the in vivo systems. Their applications have evolved the field of organoid culture to microfluidic chips with diverse cell types.
3D Culture
Scientific reports have claimed that the co-culture of retina and RPE induce adequate maturation of cone cells. Furthermore, 3D culture of these cells offer more accurate systems to study cell-cell interaction and intrinsic signaling mechanisms. They are suitable to study physiological processes and model diseases.
Personalized Medicine
The varied response to drugs has paved the way for personalized medicine. However, it requires a patient tissue cell for in vitro culture for evaluating the response and designing tailor-made treatment plans. Dedifferentiation of patient’s somatic cells iPSCs and their subsequent differentiation yield retinocytes. Therefore, iPSCs eliminate the need to isolate photoreceptors from the eye while enabling analysis of drug response.
Conclusion
Photoreceptors, also known as retinocytes, are essential for vision. Visual impairment is the result of damage or deficiency. In order to identify the signaling pathways, numerous scientists have been cultivating them in vitro. This knowledge will eventually lead to the development of therapeutics for visual recovery. The genetic engineering of these cells, their 3D culture, single-cell RNA sequencing, and regenerative medicine are accelerating the pace of ophthalmic research. Kosheeka offers human eye-derived primary retinocytes to assist in your research. The team at Kosheeka produces high-quality cells with batch consistency following robust GMP-compliant protocols. It also offers expert guidance for their in vitro culture so that scientists can focus on their core research.
FAQ’s
Q- What are Retinocytes?
Retinocytes are photoreceptors of the retina, including rod and cone cells. They receive the light signals and transmit them further. These cells are responsible for vision in daylight and at night.
Q- What is the appropriate culture medium for Retinocytes?
They can be cultivated in DMEM or neurobasal media supplemented with B27, taurine, or retinoic acid.
Q- Do Retinocytes require coating of plates during culture?
Studies have recommended that coating plates with gelatin, fibronectin, or poly-D-lysine can result in adherence and optimal growth of these cells.
Q- How are cone cells isolated from the retina?
The fovea is entirely composed of cone cells. Therefore, cone cells are extracted from this region. To obtain a pure population, MACS using peanut agglutinin lectin and opsin antibodies can be employed.



