The intricate network of blood vessels lined by endothelial cells in the human body ensures adequate blood supply to each tissue. The endothelial tissue is the barrier between plasma and tissue that controls the traffic across the tissue. Since their identification, their functional role has vastly expanded from blood flow regulation to inflammation. The significance of endothelial tissue rose from their diverse phenotypes and genotypes, exhibiting adaptation to tissue functionality. Their heterogeneity paved the way for studying the tissue-specific endothelial tissue response. This thin layer of blood vessels is also involved in different disorders, including tumors, cardiovascular diseases, and diabetes. It has spurred extensive research on these cells.
What Are Endothelial Cells (ECs)?
A thin monolayer is present towards the luminal side of vessels (the part in contact with the blood). This layer is referred to as endothelium or endothelial tissue, and the cells constituting the layer are endothelial cells. Endothelial Cells (ECs) are present in vessels, including lymphatic vessels and cardiac tissue. Although vessels also contain other cells, such as smooth muscle fibers and pericytes, the presence of ECs defines a vessel. In culture, ECs are present in polygonal morphology, displaying a cobblestone pattern.
In earlier times, it was assumed to be a static layer serving merely as a barrier. However, more studies have established the dynamic nature of endothelial tissue. Endothelial tissue can respond to diverse mechanical and chemical stimuli to maintain hemostasis.
Endothelial Cell Functions
The functions of ECs have extended far beyond the vessel lining or barrier. They now include-
- Regulation of Vascular Tone: ECs release nitric oxide (NO) and endothelin, which act on vascular smooth muscle fibers to drive vasodilation and vasoconstriction, respectively. In a healthy state, endothelial nitric oxide synthase generates NO, which relaxes smooth muscle fibers. Low NO levels lead to inflammation, abnormal blood pressure, and atherosclerosis.
- Anti-coagulation: Endothelium of blood vessels maintains an anti-coagulant surface by expressing thrombomodulin (which converts thrombin into an anti-coagulant enzyme) and tissue factor pathway inhibitor (TFPI) that prevents platelet aggregation.
- Extravasation: ECs express adhesion molecules like ICAM, VCAM, E-selectin, etc. that bind to immune cells in the bloodstream and enable their migration. Furthermore, endothelium also allows the passage of cells into the tissue by paracellular or transcellular pathways.
- Barrier: Endothelium of blood vessels modifies its permeability and regulates the movement of molecules and cells across the tissue.
- Injury Repair: ECs release von Willebrand factor (vWF) and platelet-activating factor (PAF) in case of injury to facilitate platelet activation, aggregation, and clot formation. These cells also release plasminogen activator (t-PA and u-PA)to dissolve the clot after healing.
- Angiogenesis: ECs break down their matrix, migrate, and proliferate to form new blood vessels. They release growth factors like VEGF, IGF, and FGF2 to govern the process.
- Thus, endothelial tissue is versatile in maintaining vascular and systemic health.
Types Of Endothelium Of Blood Vessels
The structure of the endothelium of blood vessels varies with its location and function. In addition to arterial, venous, and lymphatic endothelium, the three broad types of endothelium of blood vessels depend on their permeability (Fig 1).
- Continuous Endothelium: This is the most prevalent form of endothelium, where cells are tightly packed, limiting the movement of molecules across the layer (Fig 1). The classic example is the blood-brain barrier, which represents a continuous endothelium that prevents the passage of unwanted or toxic molecules.
- Fenestrated Endothelium: Fenestrae refer to pores. Pores in endothelium or fenestrated endothelium enable the easy transport of molecules across the layer (Fig 1). This type of endothelium is present in the kidney, endocrine glands, and gastrointestinal tract, and it requires extensive exchange.
- Discontinuous (Sinusoidal) Endothelium: The cells in this endothelium have gaps that allow the passage of cells (Fig 1). It could be fenestrated. The prime examples are bone marrow, spleen, and liver—tissues that filter blood and enable the migration of immune cells or progenitors.
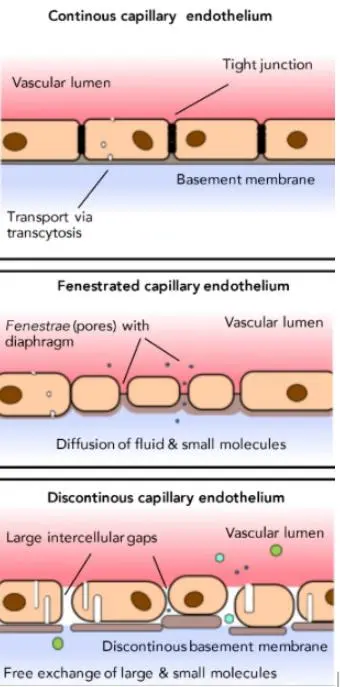
Figure 1. Types of endothelium in blood vessels (Image Courtesy: PMID: 34685692)
Applications
Cancer Research:
Vessels are an integral part of the tumor for delivering nutrients for cell growth. Therefore, tumor cells produce proangiogenic factors like VEGF to promote angiogenesis. This insight has led to the development of anti-angiogenic therapies such as bevacizumab (anti-VEGF monoclonal antibody). To enhance the delivery of drugs to the tumor microenvironment, scientists have exploited the unique nature of tumor endothelium. The disrupted tumor vasculature allows for a higher distribution of medicines in nanoforms towards tumor tissue than in normal tissue.
Cardiovascular Research:
Cardiac tissue health relies heavily on endothelial tissue. Any dysfunction in the layer can lead to atherosclerosis and hypertension. Atherosclerosis begins with lipid accumulation in arteries and the recruitment of immune cells by ECs. This process initiates plaque formation, which ruptures in the final stage, triggering thrombosis. Low NO levels in hypertension promote vasoconstriction, which frequently results in inflammation and oxidative damage. By promoting arterial remodeling, these processes cause arteries to become stiffer and lower endothelial contractility. Furthermore, myocardial infarction due to vascular occlusion can be brought on by an imbalance between coagulant and anticoagulant signals. Therefore, the development of many therapies is centered on endothelial cell research.
3D Culture:
Cell culture is evolving from two-dimensional to three-dimensional. The 3D constructs aim to represent the in vivo tissue environment better and accurately. Typically, these structures comprise only one or two cell types. However, they now incorporate ECs into the structure to facilitate blood vessels and solute exchange. The addition of endothelium has significantly enhanced the survival of these constructs. Furthermore, the development of endothelium organoids makes it possible to investigate endothelial function, malfunction, and angiogenesis in order to comprehend disease pathogenesis and create treatments.
Regenerative Medicine:
Researchers have been exploring the hematopoietic stem cell niche in bone marrow for years. Previously, only the stromal components were delineated. However, in recent years, a vascular component has also emerged. The cross-talk between stromal cells, ECs, and stem cells maintains the niche. The endothelium participates in maintaining the stem cell potency. The homing of cells into the marrow or their migration out of the tissue are under endothelial regulation.
Final Words
Endothelial tissues adapt their structure and permeability to suit the functional requirements of different tissues, highlighting their significance for physiological functions. Due to their function in immune cell migration, angiogenesis, and hemostasis, they are crucial for maintaining a healthy state. Their implication in various diseases has opened new paths for therapeutic interventions. In areas such as 3D culture and organ engineering, they aid in building vascularized tissues of the future.
Studying endothelial tissue has given rise to critical applications in biomedical science, especially in understanding disease progression, and developing therapies. By continuing to study these remarkable cells, scientists are moving closer to breakthroughs that can revolutionize medicine. Kosheeka offers endothelial cells to accelerate the pace of endothelial research. The cells are thoroughly characterized, and the Kosheeka team provides expert guidance on their in vitro culture.
FAQ’s
Q- What are endothelial cells?
These are cells that line the luminal side of blood vessels, lymphatic vessels, and the heart. They form a thin monolayer called the endothelium, a barrier between circulating blood (or lymph) and surrounding tissues. These cells are dynamic, responding to signals and stimuli to regulate blood flow, immune responses, and vascular health.
Q- What are the key functions of endothelial cells?
They perform multiple functions, including regulating vascular tone, preventing clot formation, controlling immune cell migration, regulating cell passage, repair after vessel injury, and promoting new blood vessel growth through angiogenesis. These diverse roles ensure proper circulation, inflammation control, and tissue repair.
Q- What are the different types of endothelial cells in blood vessels?
There are three main types of endothelial tissue: continuous endothelium, fenestrated, and discontinuous/sinusoidal endothelium. Each type supports the unique needs of its respective tissue.
Q- Why are endothelial cells important in research and medicine?
They are central to many areas of biomedical research. They are studied for their role in tumor angiogenesis and drug delivery in cancer. In cardiovascular health, their dysfunction is linked to atherosclerosis, hypertension, and heart disease. In 3D culture and regenerative medicine, They support vascularization, improving the survival of tissue-engineered constructs and aiding in stem cell regulation. Studying these cells paves the way for innovative therapies and biomedical breakthroughs.