Mast cells belong to the innate immune system and are vital for inflammatory and allergic responses. Their implication in diseases such as cancer, cardiovascular disorders, atherosclerosis, autoimmune conditions, etc., has prompted significant research. They regulate different aspects of physiological and pathological conditions, which has urged scientists to develop therapeutic treatments that also target these cells.
Human Mast cells
Mast cells have mononuclear morphology and contain secretory granules. Although they are known for their receptors for IgE, they also express TLRs and receptors for IgA, IgG, adenosine, C3a, etc., which are activated by PAMPs, complement proteins, and other pathogens.
The high acidity in these granules due to heparin changes the color of alkaline dyes into red-violet. This property is called metachromasia and is also present in basophils. The distinguishing factors between the two cell populations are their distinct surface markers and mast cell mononuclear morphology. They lose metachromasia after releasing granules.
Light microscopy reveals three different cell morphologies-
- Oval morphology with high quantity granules obscuring other cellular features found in subcutaneous tissue,
- Cells with lower granule quantity present in connective tissue,
- Degranulated cells which have released their granules.
Types of Mast Cells
Mast cells belong to the hematopoietic stem cell lineages. Their progenitors circulate in the blood and differentiate into mast cells once they reach the tissue. The c-kit receptor or stem cell factor (SCF) governs the differentiation process. They generally reside throughout the body in different tissues which have exposure to the external environment, such as the respiratory tract, gastrointestinal tract, etc.
Based on the composition of secretory granules, they can be classified into two subtypes- mucosal and connective tissue mast cells. The former contain tryptase in their granules and are predominantly present in mucosa. The latter have tryptase, chymase, and carboxypeptidases and are prominent near blood and lymphatic vessels located in submucosal regions or connective tissue.
Human Mast Cell Functions
Innate Immunity: Mast cells are a part of the innate immune system, thus representing the first line of defense. Their primary function is initiating inflammation. Their secretory granules contain several proteins, enzymes, and cytokines, including histamine, tryptase, tumor necrosis factor-α (TNFα), etc. Histamine promotes smooth muscle constriction, leukocyte migration, and vascular permeability. Cytokines also affect the tissue functions to alleviate pathogen burden, such as increased mucus production. Heparin, tissue-plasminogen activator (t-PA), and tryptase alter the blood flow in favor of immune cell chemotaxis.
In addition to granular content, they also consist of other mediators from de novo synthesis, such as prostaglandins, leukotrienes, IL10, etc. They also produce antibacterial substances such as defensins, cathelicidins, etc. These cells are essential for the differentiation of follicular helper T lymphocytes, dendritic cell activation, and maturation of IgA. They also activate cytotoxic T lymphocytes to mediate antiviral response.
Wound Repair: Upon injury, mast cells secrete procoagulant cytokines and heparin, thus supporting the repair processes. They also release angiogenic proteins such as VEGF, TGFβ, IL8, TNFα, and FGF2 that assist in angiogenesis. Research has also suggested their role in wound contraction and nerve regeneration.
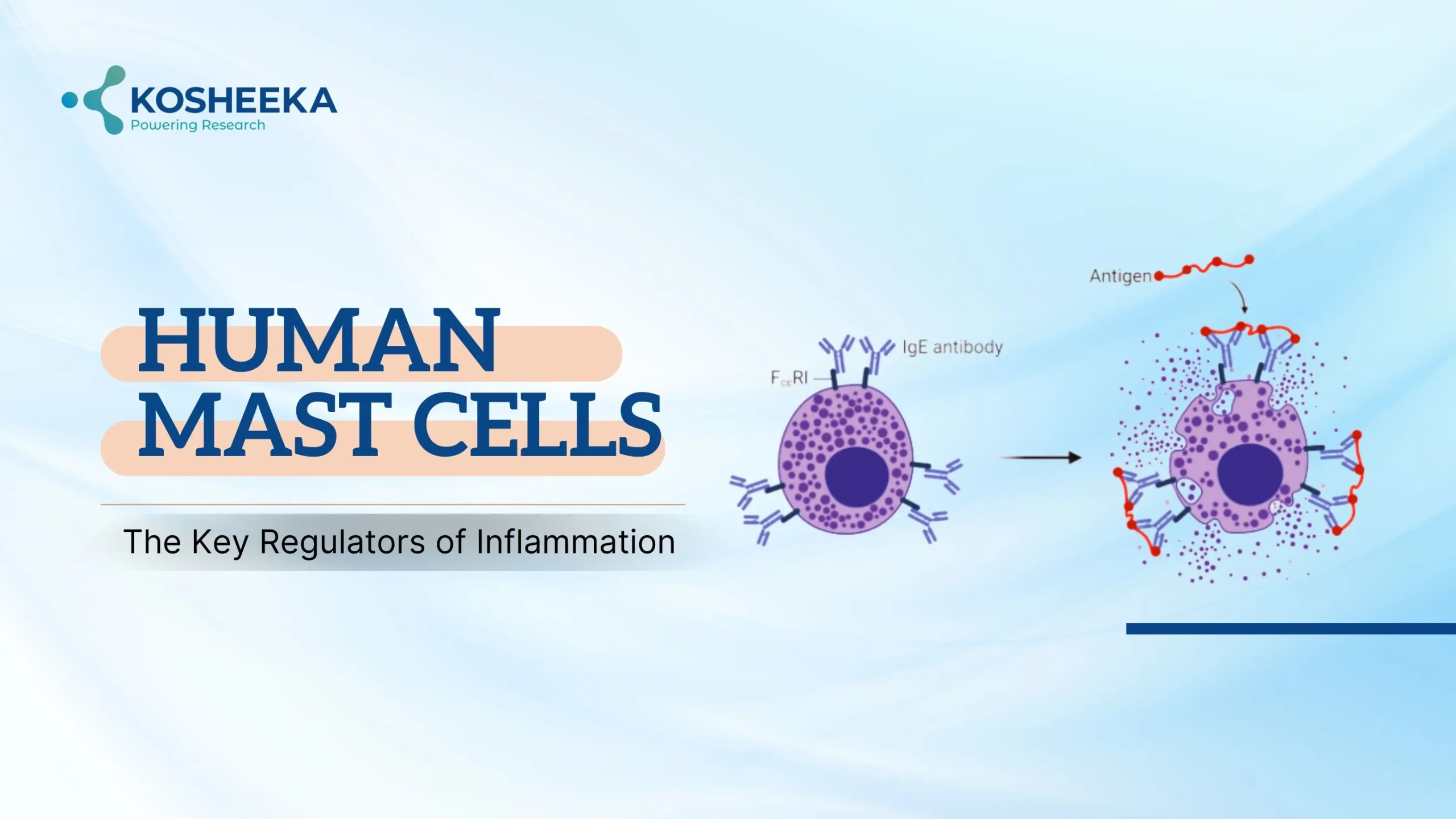
Degranulation Process
B lymphocytes produce IgM and IgD before activation. After the antigen initiates the immune response, activated Th2 lymphocytes release cytokines like IL4, which switches the antibody class from IgM to IgE. IgE binds to its receptors—FCϵRI on mast cell surface—and only a small amount of IgE remains in a soluble state. The antigen binds to the IgE, cross-linking the membrane receptors and triggering degranulation.
Degranulation occurs in two manners- anaphylactic degranulation involves the release of complete granular content, whereas piecemeal degranulation shows the release of a certain amount of granular content in a slow and graded manner. The type of pathogen also defines the mast cell response. For instance, gram-positive bacteria stimulate the release of cytokines without degranulation, whereas peptidoglycan causes degranulation and histamine secretion.
Signaling Mechanisms of Activation
FCϵRI comprises α-chain (binds to IgE), β-chain (spans the transmembrane region), and ϒ-chain (disulfide-linked homodimer). Both β and ϒ chains have ITAM motifs. Cross-linking receptors activate Lyn tyrosine kinase, which phosphorylates tyrosine on ITAMs. Syk tyrosine kinases bind to ITAMs, which triggers their phosphorylation. Syk, in turn, phosphorylates and activates the linker for activation of T cells-1 (LAT1) and LAT2.
Binding to LAT proteins, phosphorylates and activates PLCϒ, which hydrolyzes phosphatidylinositol-4,5-bisphosphate (PIP2) to inositial-3,4,5-triphosphate (IP3) and diacylglycerol (DAG). IP3 stimulates calcium efflux from the endoplasmic reticulum to the cytoplasm. The increased calcium levels translocate NF-κB into the nucleus, resulting in the transcription of IL6, IL13, and TNFα.
FCϵRI also activates Fyn, an Src kinase, which activates PI3K. PI3K converts PIP2 into phosphatidylinositol-3,4,5-bisphosphate (PIP3), which recruits and activates Akt. It activates the mTOR signaling pathway, resulting in mast cell chemotaxis of and the production of cytokines.
Clinical Relevance
Type I Hypersensitivity: The tissues employ VCAM1 and CXCR2 to recruit mast cells by their cell surface integrin- α4β7. In the respiratory tract, they cause mucus secretion, airway constriction, and increased vessel permeability, leading to congestion, nasal obstruction, and asthma. A similar cascade leads to rhinitis, hives, and anaphylaxis. Antihistamines are usually employed to treat this disorder.
Mastocytosis: It refers to the abnormal mast cell proliferation, resulting from an activating mutation of c-kit receptor. The condition increases the inflammatory mediators, primarily affecting the skin, gastrointestinal system, and bone marrow. However, it can also occur in other organs, leading to their dysfunction.
Anti-Parasitic Response: Mast cells were first recognized for their anti-parasitic response. In the gastrointestinal tract, their activation results in edema, smooth muscle contraction, and increased vascular permeability, leading to vomiting and diarrhea, which remove the parasite from the body. The coughing is also a similar response in the respiratory tract that propels the pathogen out.
Cancer Therapy: Research has associated poor treatment responses with mast cells in tumor microenvironment. However, their capacity to support or inhibit the tumor microenvironment depends on the type and stage of the tumor as well as mast cell activation and location in tumor microenvironment. Mast cell TNFα causes tumor cytotoxicity, whereas tryptase activates matrix metalloproteinases that degrade extracellular matrix, promoting tumor growth. The effect of histamine depends on the receptor they interact with. Treatment that can target c-kit, like imatinib, nilotinib, dasatinib, etc., can prove beneficial in regulating mast cell numbers and tumor cell survival.
Conclusion
Mast cells use a variety of cytokines and enzymes to mediate immune responses. They cause clinically significant physiological alterations in response to infections or foreign particles. These cells can serve as therapeutic targets as the increasing research studies on them reveals their involvement in the pathophysiology of various illnesses. Kosheeka delivers the human mast cells to accelerate these discoveries and subsequent drug development. Our team rigorously characterizes and tests the product to ensure its viability and purity.
FAQs
Q: What are mast cells?
They are tissue-resident immune cells with mononuclear morphology derived from hematopoietic stem cell lineage in bone marrow.
Q: What are mast cell functions?
They release inflammatory mediators in response to foreign particles or pathogens. These mediators recruit leukocytes by promoting chemotaxis and vessel permeability to eliminate the pathogen. Furthermore, they produce antimicrobial peptides and support injury repair.
Q: What are the signaling pathways behind degranulation?
The cross-linking of the IgE receptor on the mast cell surface activates several tyrosine kinases and include activation of ITAM motifs on the receptor, ultimately leading to PLCϒ pathway. Additionally, they also follow the PI3K/Akt/mTOR pathway.
Q: Do mast cells support tumor growth?
They can show both anti-tumorigenic and tumorigenic properties. However, their response varies depending on the type of tumor and mast cell location in the tumor.