Human skin-derived dermal fibroblasts maintain skin homeostasis and support its functions. Although overlooked before, the advances in the dermatological field have put them into the spotlight. They produce skin extracellular matrix proteins like collagen and elastin, conferring elasticity and refined texture to the skin. Their role in wound healing, aging, and melanogenesis has been researched. Additionally, they have found application in regenerative medicine.
Human Skin-Derived Dermal Fibroblasts
Skin comprises two layers- the outer epidermis and the inner dermis. Dermis is further divided into papillary and reticular layers. Fibroblasts are the primary dermis cells. Rudolf Virchow was the first to recognize them, and Ernest Ziegler described them as cells producing the connective tissue in a wound. Gradually, research studies expanded on their role.
They also participate in the proliferation and differentiation of epithelial cells or keratinocytes. Derived from mesoderm, they share similarities with mesenchymal stem cells. Epithelial cells via epithelial-mesenchymal transition to fibroblasts. Interaction between fibroblasts and keratinocytes is responsible for the varying types of skin on the foot and palm, as per research results. Fibroblasts also express pattern recognition receptors to mount an immune response against pathogens.
The Isolation Procedure
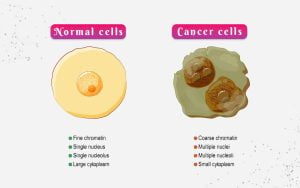
For the separation of human skin-derived dermal fibroblasts, a thin section of skin is sliced. The isolation process is a two-step procedure employing the enzymatic digestion method. The first step separates the dermis and epidermis layers of skin by overnight incubation in dispase enzyme. The second step requires incubation of the dermis in collagenase solution, which isolates fibroblasts. Their culture medium is DMEM or F-12 medium, along with supplementation with factors such as FGF2, hydrocortisone, and ascorbic acid 2-phosphate. They show spindle morphology and have identification markers – platelet-derived growth factor (PDGFR) α, PDGFRβ, and CD90. Transcriptional profiling has identified two different subsets of these cells- papillary and reticular fibroblasts, each with distinct gene expression and functions.
Applications
Wound healing
Tissue repair and wound healing are dynamic processes. Fibroblasts are the key cellular players of the process vital in each of its phases. In brief, injury triggers platelet clotting, immune cell recruitment, and fibroblast migration. Fibroblasts strengthen the immune response by enhancing the survival, migration, and proliferation of immune cells. They remodel the ECM by secreting ECM proteins and matrix-degrading metalloproteinases. They release angiogenic factors for vessel formation. In the last phase, they transdifferentiate into myofibroblasts that drive wound closure and ECM modeling.
Any deregulation of the process can result in chronic wounds found in diabetic ulcers, venous foot ulcers, keloid scarring, etc. Since fibroblasts are the integral component of the healing process, extensive research is conducted on them to elucidate the signaling pathways working behind the process. The research can facilitate the discovery of therapeutic targets for drug development. For example, the use of anti-inflammatory drugs to inhibit fibroblast activity.
Regenerative Medicine
The recognition of transcription factors for pluripotency and murine fibroblast reprogramming into stem cells, known as induced pluripotent stem cells (iPSCs), has been the most remarkable breakthrough of the last century. Since then, iPSCs have become a favored source of stem cells. They can be easily extracted from adult tissue, dedifferentiated, and redifferentiated into desired tissue cells. Dermal fibroblasts have become the preferred source due to their easy availability and painless extraction.
Furthermore, these cells also exhibit stem cell-like properties. They have demonstrated chondrogenic differentiation. A study by Chee et al. showed regeneration in the intervertebral disc of mice after fibroblast transplantation. These cells even display multilineage differentiation into adipocytes, osteocytes, neural cells, Schwann cells, smooth muscle cells, hepatocytes, etc. Their phenotype is similar to mesenchymal stem cells (MSCs). Their easy isolation and higher proliferation rate also offer a cost-effective alternative to MSCs.
Artificial Skin
Artificial skin has captivated the interest of scientists after witnessing the positive effects of fibroblast transplantation on wrinkles and acne scars. It employs an ECM or a scaffold for cell cultivation and the creation of a skin substitute. For example, Apilgraf constitutes foreskin neonatal fibroblasts on a bovine type I collagen along with foreskin neonatal keratinocytes. It was approved for venous leg ulcers and diabetic foot ulcers for effective wound healing.
Biobrane is another such product that contains only a scaffold comprising nylon mesh, collagen peptides, and silicone membrane. Host wound fibroblasts supply it with growth factors to promote epidermalization. After healing, the product is removed. Transcyte combines cells, a scaffold, and growth factors. Several such products have entered the commercial landscape, including LAVIV, Transcyte, Isolagen, Dermgraft, etc. However, dermal regeneration was evident with scaffolds containing fibroblasts. It indicates that wound healing requires these cells.
Aging
Dermal fibroblasts secrete factors keratinocyte growth factors 1 and 10 (KGF-1 and KGF-10, also known as KGF-2), granulocyte-macrophage colony-stimulating factor (GM-CSF), epidermal growth factor (EGF), interleukin 6 (IL-6), etc. These factors govern the differentiation and proliferation of skin epithelial cells or keratinocytes. They also promote migration and proliferation of endothelial cells for the stabilization of blood vessels. They also stimulate the melanogenesis process responsible for skin pigmentation.
Aging changes two key mechanisms involving dermal fibroblasts. Firstly, aging decreases their number. Their progenitors and differentiated counterparts decline. They undergo senescence and cell cycle arrest. These senescent cells degrade ECM and trigger inflammation. Therefore, the strategies for anti-aging skin therapies focus on fibroblasts or their functions. For instance, retinoids modulate gene expression to increase ECM synthesis and decrease ECM breakdown by matrix metalloproteinases. Laser therapy affects dermal fibroblasts to regenerate skin.
Product-Related Queries, Or Partnership Inquiries
Diseases
Autoimmune skin diseases such as vitiligo, psoriasis, atopic dermatitis, etc., impact numerous people across the world due to immune system malfunction. Many studies have indicated that dermal fibroblasts from psoriatic skin have a distinct genetic profile. The genes for inflammation and chemotaxis were upregulated in these cells. In dermatitis, they increase interaction with mast cells and keratinocytes to impair the barrier structure and function. The cytokine IL22 binds to its receptors on fibroblasts and shows elevated levels in the skin of dermatitis patients.
In vitiligo, these cells promote recruitment and retention of leukocytes. These cells also support inflammation in scleroderma. Therefore, many therapies have directed their efforts on fibroblast pathways. For instance, IL17 activates fibroblasts thus, IL17 antibody brodalumab can treat fibrosis. Similarly, IL23 inhibitor effectively treat psoriasis.
Conclusion
Dermal fibroblasts are essential components of skin. They orchestrate wound healing, keratinocyte proliferation, and immune response. Treatment options for dermatology have expanded due to its use in anti-aging treatments. Research on these cells has exploded due to their participation in skin disorders and chronic wound healing. The ability of these cells to regenerate is also creating new opportunities for stem cell treatments. Kosheeka supplies human skin-derived dermal fibroblasts belonging to diverse species such as human, rat, swine, and mouse. Our team thoroughly characterizes them and runs stringent quality tests to ensure a pure population of cells for reliable research.
FAQs:
Q – What is the primary function of dermal fibroblasts?
They secrete proteins such as collagen and elastin that constitute the extracellular matrix of the skin; thus, these cells maintain the architecture and function of the skin.
Q – What are the types of dermal fibroblasts?
Although there are several types of dermal fibroblasts, they are broadly classified as papillary and reticular fibroblasts.
Q – How do dermal fibroblasts regulate wound healing?
They induce matrix modeling, angiogenesis, and enhance immune response. They also transform into myofibroblasts that drive wound closure.
Q – What are the applications of dermal fibroblasts in regenerative medicine?
They can be reprogrammed into induced pluripotent stem cells. They also exhibit mesenchymal stem cell-like properties and differentiate into multiple cell types.