One of the major causes of acute kidney injury (AKI) is sepsis: this becomes significant given that 1–35% of hospitalized patients develop AKI. In the case of general surgery, the incidence of AKI is close to 1% but this figure reaches a whopping 70% for critically ill patients accounting for in-hospital mortality of 50% in the case of multi-organ failure! (Zarbock et al, 2014).
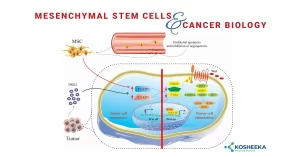
While the exact mechanisms of this condition are yet to be unraveled in detail, the following 3 mechanisms have been shown to be involved in this: aberrant cell bioenergetics and renal microcirculation as well as inflammation. Research shows the immunomodulatory properties of mesenchymal stem cells (MSCs), especially in terms of lowering the molecules involved in inflammation, MSCs have been used in several studies to treat sepsis-associated AKI.
2014-published research by Luo and team reported the promise of using MSCs to treat in the C57BL/6 mice model. The administration of MSCs lowered the levels of serum creatinine and blood urea nitrogen levels. The levels of the molecules IL-6, IL-17, tumor necrosis factor α, interferon γ, CXCL1, CXCL2, CXCL5, CCL2, and CCL3 were all also lowered. The injection of MSCs caused the lowering of bacterial loads in the blood and neutrophil infiltration in the kidney. Overall, the survival rate of the animals that received MSCs was higher than that of the controls (saline treatment group).
Scientists Cóndor and team showed the protective role of human Wharton’s jelly-derived mesenchymal stem cells in sepsis in a rat model of sepsis. The rationale behind the experiments was that these MSCs are known to lower the levels of proinflammatory cytokines and apoptosis markers. One of the factors involved in sepsis-induced acute kidney injury is reduced levels of a protein called Klotho. The administration of MSCs boosted the levels of Klotho and other factors such as vascular endothelial growth factor. The glomerular filtration rate (GFR) that was reduced in the rat models was also improved along with an improvement in tubular function. The level of apoptosis was lowered in the kidney and the overall survival was improved showing the protective effects of MSCs in sepsis.
Given the seriousness of sepsis in intensive ward units and its grim figures, the quest is to search for a suitable and effective approach to address this condition. MSCs on account of their availability from a broad range of cells, limited ethical challenges and their ability to modulate the immune system are a promising approach to treat this critical condition.
References:
Zarbock, A., Gomez, H., & Kellum, J. A. (2014). Sepsis-induced acute kidney injury revisited: pathophysiology, prevention and future therapies. Current opinion in critical care, 20 (6), 588–595.
Horák, J., Nalos, L., Martínková, V., Beneš, J., Štengl, M., & Matějovič, M. (2017). Mesenchymal Stem Cells in Sepsis and Associated Organ Dysfunction: A Promising Future or Blind Alley? Stem cells international, 2017, 7304121.
Luo CJ, Zhang FJ, Zhang L, Geng YQ, Li QG, Hong Q, Fu B, Zhu F, Cui SY, Feng Z, Sun XF, Chen XM. Mesenchymal stem cells ameliorate sepsis-associated acute kidney injury in mice. Shock. 2014 Feb; 41(2):123-9.
Cóndor, J. M., Rodrigues, C. E., Sousa Moreira, R. d., Canale, D., Volpini, R. A., Shimizu, M. H., Camara, N. O., Noronha, I., & Andrade, L. (2016). Treatment With Human Wharton’s Jelly-Derived Mesenchymal Stem Cells Attenuates Sepsis-Induced Kidney Injury, Liver Injury, and Endothelial Dysfunction. Stem cells translational medicine, 5(8), 1048–1057.