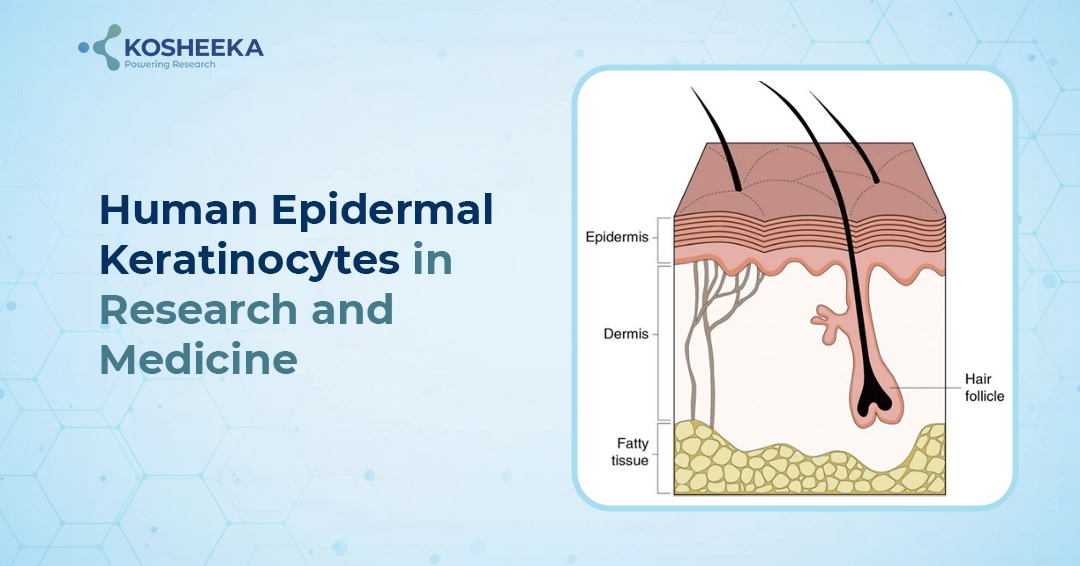
Human Epidermal Keratinocytes (HEK) are ideal cell platforms to study wound healing, toxicology, skin biology/diseases, human papillomaviruses (HPV) infection, regenerative medicine and dermatological/cosmetic research. HEKs are also used as in vitro human skin models to evaluate anti-inflammatory effects of cosmetic formulations. Epidermis, the outermost skin layer, is composed of 90% HEK. It acts as a physical barrier, the intermediate filament keratin. Keratinocytes receive melanin from melanocytes and store it for protection from UV radiation. HEK cells are either primary cells isolated from tissue biopsies or can be derived from induced pluripotent stem cells (iPSCs).
Primary Human Epidermal Keratinocytes (HEK)

HEKs are generally isolated from human skin tissues from surgical waste materials with donor consent. HEKs are isolated by enzymatic treatment with dispase or trypsin after separating epidermis from dermis. It can also be isolated by explant culture methods. Isolated keratinocytes are cultured in specific media with growth factors e.g. keratinocyte growth factors (KGF), Epidermal Growth Factor (EGF) etc. This specialized media supports proliferation and maintenance. HEK also required a feeder layer or surface coating for enhanced cell attachment and growth.
iPSC-Derived Keratinocytes
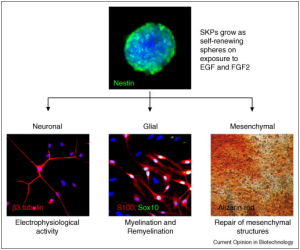
Induced pluripotent stem cells (iPSCs) are generated from human somatic cells e.g. Peripheral Blood Mononuclear Cells (PBMCs), fibroblast etc. using Yamanaka factors OCT4, SOX2, KLF4, C-MYC. iPSCs are sequentially differentiated towards keratinocytes using growth factors and signaling molecules through ectodermal lineage specification by mimicking embryonic epidermal development.
Characterization of HEK

- Morphological Analysis: HEK exhibits a cobblestone-like morphology.
- Molecular characterization: Expression of specific keratinocyte markers such as Keratin 5, Keratin 14, Keratin 10, and Keratin 1 is assessed using immunocytochemistry and flow cytometry. Involucrin, Loricrin, and filaggrin also confirm the differentiated phenotype of HEK. α6β4 integrin and E-Cadherin also play a crucial role in maintaining the integrity of the epidermal layer.
- Functional Characterization: Barrier function assay is used to assess the integrity and permeability of the keratinocyte layer.
Applications of HEK
- Disease Modeling: HEK and iPSC-derived keratinocytes are used to study disease mechanisms and their therapeutic interventions by various skin disease modeling, e.g. psoriasis, atopic dermatitis, eczema, epidermolysis bullosa etc.
- Drug Screening and Toxicology: Keratinocytes serve as a model for efficacy, toxicology and safety assessment of dermatological drugs, cosmetics and other topical ointments.
- Regenerative Medicine: Keratinocytes are used to generate skin grafts to treat chronic wounds like burns and other skin injuries.
- Gene Editing and Therapy: CRISPR/Cas9 editing tools are used to treat various genetic skin disorders, e.g. Ichthyosis, vitiligo etc.
- Personalized Therapy: iPSCs-derived keratinocytes enable facilitating personalized therapeutic strategies, improving treatment outcomes.
Conclusion
HEK are invaluable tools in dermatological research and regenerative medicine. Their ability to model diseases, screen drugs, and contribute to personalized medicine underscores their significance. At Kosheeka, we are committed to advancing these technologies to support groundbreaking research and therapeutic developments. HEKs are amenable to high throughput drug screening for toxicology and safety studies. For more information about our customized cell culture services and to learn how we can support your research needs, please contact us.